Worst Case for Women
The pandemic exacerbates the effects of Trump's anti-woman foreign policies

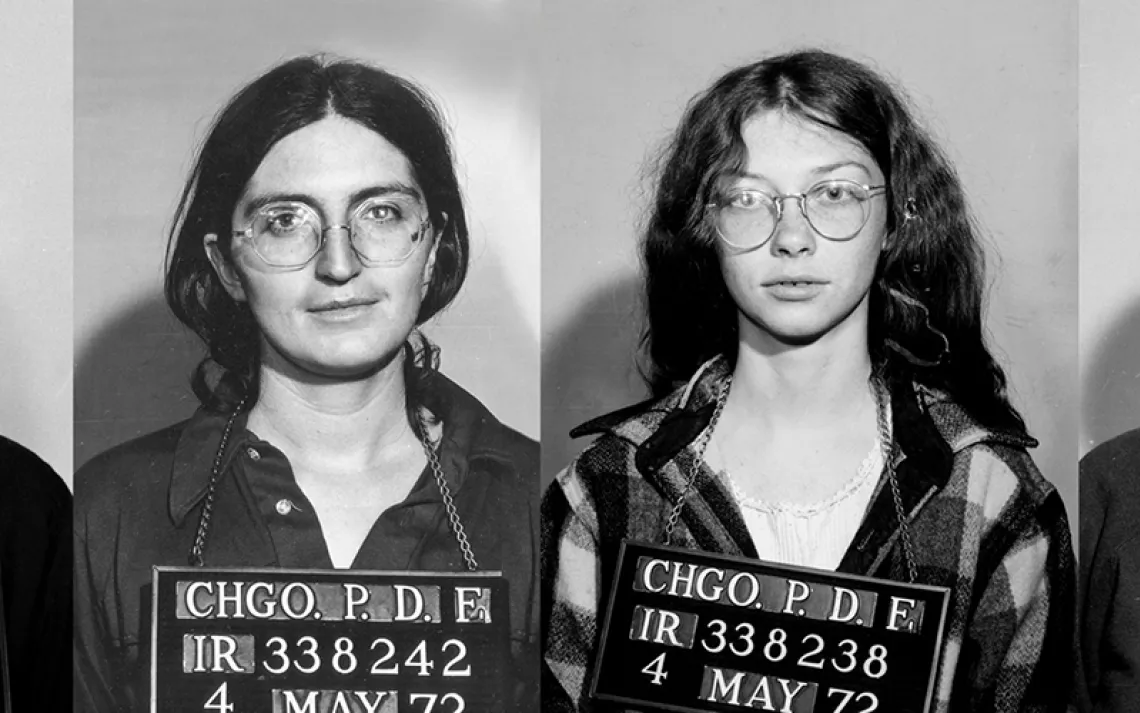
Sedalia do Rego, left, of the Bairo Pite Health Clinic in Dili, and Bana Rosa, right, talk with a woman who is pregnant with her second child in rural East Timor. | Photo by Jerry Redfern
COVID-19 has many ways to kill, not all of them obvious. For the women of the world, the pandemic is obstructing access to health care, and experts predict catastrophic outcomes: women and girls having babies they don’t want and abortions that kill them, mothers dying in childbirth, and newborns succumbing to treatable diseases. Worsening the situation are the destructive effects of US foreign policy.
“The worst-case scenario is playing out now,” says Jonathan Rucks, senior director of policy and advocacy for the reproductive health and rights group PAI.
Rucks points to one of President Donald Trump's first moves when he took office in 2017: reinstating the on-again, off-again “Global Gag Rule,” which prohibits NGOs that receive US health-care funding from providing abortion services, referrals, counseling, or advocacy. Ronald Reagan first implemented the policy in 1984; every subsequent Democratic president has repealed it, and every Republican has restored it. Previous iterations of the gag rule applied only to reproductive and family planning programs, but Trump expanded the policy several steps further to cover nearly all US global health funding—$12 billion worth of programs ranging from HIV/AIDS to tuberculosis, nutrition, infant and maternal health, malaria, and more. He forced NGOs to choose whether to take US funding and abide by the rules or decline the money and make do. His administration named the program “Protecting Life in Global Health Assistance.”
"The Global Gag Rule closed clinics, closed service delivery sites, and cut off services to vulnerable and key populations out in rural areas,” Rucks says. According to GAO research published in March, 54 projects worldwide declined more than $150 million in US health funding in 2017 and 2018. Some of the affected programs were women’s sole access to health care of any kind.
Now, the response to COVID-19 places even greater constraints on populations hardest hit by the gag rule. Worldwide, women are losing access to reproductive health care due to lockdowns, clinic closures, diverted resources, and disruptions in transportation. The Guttmacher Institute, a reproductive health research group, estimates that even a 10 percent reduction in access to health care during the coronavirus pandemic could result in 15 million unintended pregnancies, 28,000 maternal fatalities, and the deaths of 168,000 newborns.
“The gag rule and this COVID—they are two faces of the same coin,” says Abebe Shibru, Zimbabwe country director for Marie Stopes International (MSI). The organization's Zimbabwe programs were initially cut in half, from 1,200 sites to 600, when MSI declined US funding under Trump’s restrictions. COVID-19 exacerbates the effects of already limited services, Shibru says.
In Zimbabwe, a national lockdown implemented on March 30 and extended on May 1 has restricted movement nationwide, and MSI’s mobile health teams can no longer reach remote sites. Instead, women are told to meet MSI workers at public facilities, but “they are afraid of security and the police,” Shibru says. Even though health care is considered essential, authorities are stopping women en route to clinics, asking where they are going and escorting them home if they don’t show proof of medical need. MSI has started sending appointment notices to women’s mobile phones—but that only works for women with phones.
MSI Zimbabwe’s client visits are down by 70 percent, Shibru says, but “women are not in a position to lock down their uterus. Because they are not the decision-maker in the marital relationship.” He expects three things in the coming months: a baby boom, unintended pregnancies resulting in unsafe abortions, and abortions ending in maternal deaths.
Ebola offers a view of the future. During the 2013–2016 outbreak, says Shannon Kowalski, the International Women’s Health Coalition director of advocacy and policy, “We saw devastating consequences for women and girls.” Governments diverted funding from women’s health care. Maternal and infant deaths spiked, as did teen pregnancy and child marriage. Many girls who left school never went back. And the risk of sexual assault increased dramatically. “Violence tends to exacerbate in moments of stress,” Kowalski says, and a lockdown can be “when relationships turn violent for the first time.” It’s critical to keep hotlines and shelters open, she says, so women’s access to help isn’t shuttered.
Sexual and reproductive health care should be central to pandemic responses, Rucks says, “because women and girls need access to those vital services all the time.” But the past three years have brought the opposite. “We’ve seen attacks on global sexual and reproductive health and rights from every corner of this administration,” says Seema Jalan, executive director of the Universal Access Project and Policy at the United Nations Foundation. “One of the most harmful and shortsighted decisions was to eliminate US funding for the UN Population Fund.” That happened in 2017 and had continued every year since. Since the pandemic hit, several US states have used COVID-19 as a reason to block abortion access. And on April 14, President Trump announced he was halting more than $400 million in funding for the World Health Organization.
That’s another disaster, says Shibru. “When it comes to Africa, we are very resource-scarce,” he says. “For health, we are mostly dependent on WHO and WHO-related organizations.” The recent US cuts mean more child and maternal health funds will be diverted to fight COVID-19, and consequently, more women and children will die.
If there is an upside to this crisis, says Kowalski, it's that it offers an opportunity “to reimagine what primary health care should look like after this crisis subsides.” Governments can make critical changes now, before the next pandemic hits: Use telemedicine to reach women remotely, invest heavily in midwifery and safe home deliveries, and make contraceptives like the pill available over the counter. “Women are quite able to make a safe determination about whether or not they need contraceptives,” she says. “There’s no reason why we need to maintain barriers.”
COVID-19 is also a wake-up call for developing nations to reduce dependency on American and European donors, Shibru says. African countries should invest more of their own budgets in critical health care. “We have never encountered a pandemic with this level of magnitude,” he says. “Africa should prepare itself for another round of catastrophe.”
 The Magazine of The Sierra Club
The Magazine of The Sierra Club