Two Pandemic Years Have Created a PPE Wasteland
So where do we go from here?
Between disinfecting my groceries and navigating a newsfeed overflowing with sourdough bread and Tiger King memes, empty store shelves, PPE shortages, soaring COVID-19 cases, a devastating death count, and the macabre notion that a global pause on commerce could help heal the planet, I received a package from a friend during the frenzied lockdown of March 2020. A box of homemade masks.
Like so many people, my family wore and washed our fabric armor for over a year, the masks’ once-bright colors and floral prints fading as the months passed. Last fall, however, the emergence of the Omicron variant, with its high transmissibility, changed the way we safeguarded ourselves from the pandemic. Respirators, the highest form of protection, became the norm, discarding a last shred of sustainability we could cling to in the face of a virus that has taken so much from all of us. Understandably, two years’ worth of COVID-19 has amassed a behemoth amount of plastic, and proved a tremendous setback to waste-reduction efforts across sectors.
It's no secret that PPE use has skyrocketed since the pandemic’s onset. We used an estimated 4.5 trillion face masks in 2020 alone, while 65 billion single-use gloves have been trashed monthly throughout the pandemic. Most have ended up in landfills, incinerators, and an already taxed environment, contributing to over 8 million tons of pandemic-related plastic waste.
Not surprisingly, health-care settings—which already struggled with waste management—have contributed enormously, accounting for nearly three-quarters of all ocean-bound pandemic plastic. Though the industry is far from isolated.
“The volumes of waste increased on average by three to four times in health-care facilities. In some places it increased by 10 times,” says Dr. Maggie Montgomery, a technical officer with the World Health Organization (WHO) and lead author of a recent report that found most of the 87,000 tons of personal protective equipment distributed by the UN from March 2020 to November 2021 wound up as trash.
Most surprising? Almost half of all PPE distributed by the UN was nonessential—meaning health-care facilities worldwide have unnecessarily used and discarded tons of personal protective equipment. The overflow was largely due to initial unknowns about the virus, such as its survivability in the environment and how it’s transmitted. This led many countries and facilities to use excessive amounts of PPE, and to mistakenly deem up to 100 percent of used equipment as hazardous (only 10 to 15 percent of which should have actually been classified as such, the WHO report states).
The Issue of Medical Waste
Despite the extraordinary circumstances, the problem of waste management in medical settings is not new. Pre-COVID-19, 30 percent of health-care facilities (and twice that amount in the least-developed countries) struggled to cope with existing waste streams. At the time, plastic constituted 25 percent of hospital waste. Today, it accounts for at least half of all health-care waste, according to Montgomery.
Supply-chain disruptions, recycling shutdowns, fear of coronavirus infection, improper disposal, and overuse of PPE have only exacerbated the issue. A lack of foresight as to how the influx of waste generated by increased PPE production would be managed, recycled, and reused, has played a pivotal role in the problem.
“We saw a lot of investments happening on the PPE side, on the vaccine side, on the testing side,” Montgomery says. “None of these investments were thinking, ‘How are we going to handle all the waste?’”
We’ve all seen masks and gloves strewn across pavement, puddles, and sand, but personal protective equipment extends beyond these most visible applications of PPE waste to include surgical gowns, hair and beard nets, shoe covers, plastic wrap, shields, sheeting, sanitizing equipment, garments, test kits, and more. This influx of plastic-based, hard-to-recycle PPE has been a substantial impediment to waste-reduction efforts worldwide. Yet it’s only one part of the mountain of trash generated by the pandemic.
COVID-19 and Plastic
Plastic production has more than doubled since COVID’s earliest days, a deluge compounded by the halting of existing efforts to reduce, reuse, and recycle internationally as governments, companies, and individuals shifted priorities and clamored to address growing infection rates and corresponding sanitation concerns.
In 2020, hard-won plastic bag bans in states across the nation were suddenly put on hold. Supermarkets, restaurants, retailers, and other institutions that had long worked to reduce single-use plastics reverted to disposable bags, straws, take-out containers, and other forms of plastic packaging to protect their communities.
Unfortunately, all this emphasis on public safety has missed a critical element: the impact on environmental health. Two years after that memorable March 2020 lockdown, and tons of PPE pollution later, where do we go from here?
“What’s the number one way to reduce these volumes?” Montgomery asks. “Don’t use what’s not needed. Gloves are not needed, even by health-care providers for the majority of COVID-19 interactions. They’re not needed for vaccinations. They’re not needed for simple consultations. They’re not needed for testing. But yet we see gloves being used a lot.” (The CDC concurs, advising that in most situations, like grocery shopping and running errands, the public does not need gloves to protect themselves from COVID-19.)
“We see that there’s a real behavior element around [the idea] that more is better, and more is safer,” says Montgomery. “It doesn’t necessarily make the health-care workers safer, and we know there’s a lot of repercussions in how that waste then needs to be handled and treated.”
Those behaviors have been a challenge to change, from health-care to the public sector, and will require proactive educational efforts across industries. But the strategies don’t have to be complicated. Successful initiatives like England’s “The Gloves Are Off” campaign, a training program that resulted in reduced glove use in health-care settings pre-pandemic, can provide a helpful model, Montgomery notes.
Travis Hawks, sustainability specialist for Advocate Aurora Health, a US-based nonprofit with over 500 health-care sites and a member of the Healthcare Plastics Recycling Council’s advisory board, confirms the need to resume working toward waste-reduction goals. “Many noncritical efforts were put on pause to focus on the COVID crisis,” Hawks wrote in an email. “We’re now slowly reengaging team members in efforts around recycling.” Those efforts include, “continuing our focus on education to reduce contamination of our [waste] streams, education for recyclers on differences between infectious waste (IW) and non-IW items they can accept, and engagement with our sites to reduce any unnecessary single-use plastic items.”
In addition to reducing the amount of PPE that’s being used globally, reusing PPE is another huge area for growth. The demand for single-use masks poses one of the largest opportunities for improvement—a need that’s been highlighted by governmental masking recommendations around the Omicron variant, including mandates that specific types of masks be used.
Though safe and reusable high-quality masks exist, they’re currently more costly and often not readily available in stores. Increasing public awareness about these options, along with incentives to purchase reusables, could go a long way toward eliminating future waste, Montgomery says.
The development of reusable gloves and other often used forms of PPE, in tandem with an emphasis on decreasing plastic packaging of nonsterile protective equipment, are additional key areas of improvement. “Health care can reprocess and reuse certain PPE through sterilizing the items following CDC guidelines,” Hawks adds, highlighting another conservation strategy.
How to Ramp Up Recycling?
The dire need for global investment into recycling of health-care waste is an issue felt most acutely in developing countries where waste management is already of pressing concern. The pandemic poses an opportunity to bring such endeavors to fruition.
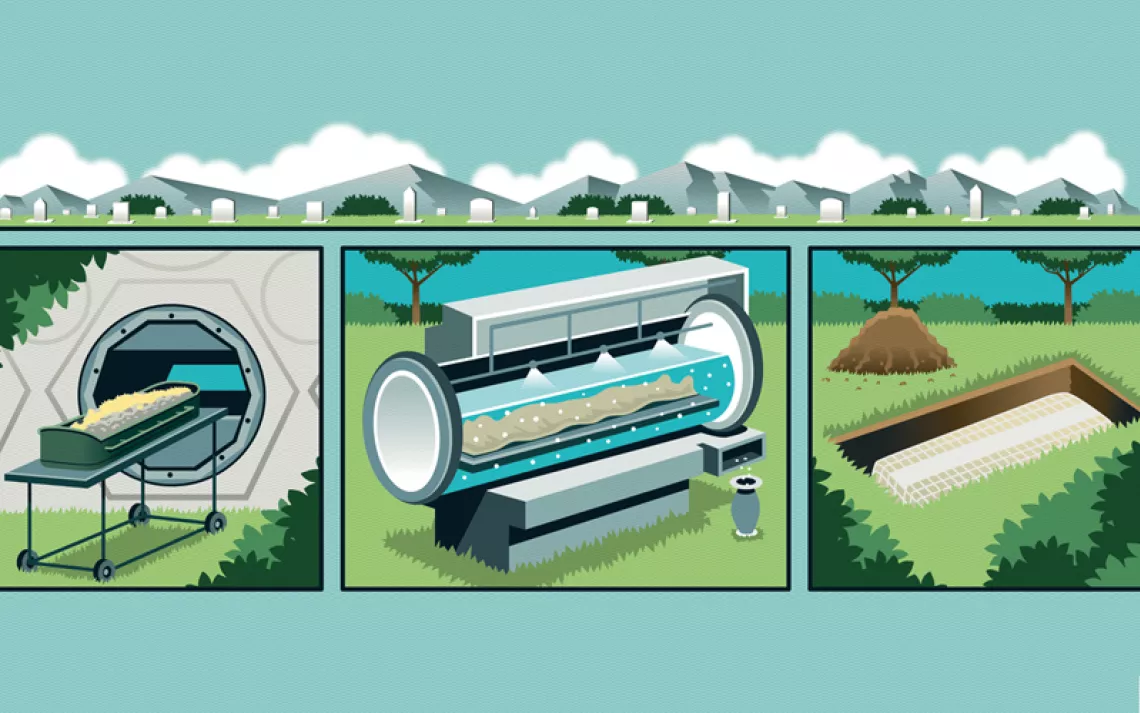
Fortunately, efforts to recycle PPE are already underway worldwide. Terracycle is one such company working to recycle gloves, masks, and other forms of PPE used outside of health-care settings through its Zero Waste Box program, which transforms used materials into new products, such as plastic pellets, lumber, decking, flooring tiles, outdoor furniture, and more, with the help of third parties. Globally, PPE is also being converted into construction bricks, road-building materials, and even batteries.
There is momentum behind pyrolysis as well, a waste-to-energy temperature reaction that reduces PPE to chemicals, resins, oil, propane, ethylene, and other fuels. (Though promoted by industry as a sustainable solution to waste reduction for its potential to decrease landfilling, emissions, and fossil fuel extraction, the process remains controversial, with opponents considering it little more than a costlier incineration method—one that could actually increase emissions and generate toxic waste.) In addition to recycling, manufacturers can continue to reduce waste by developing new PPE from biobased, renewable, recycled, and recyclable materials.
Of course, these essential waste-reduction efforts will require buy-in from industry, government, and individuals. Governmental agencies can help foster solutions by investing in sustainable alternatives and building essential recycling systems, reviewing and recommending new products as they come to market, and promoting adoption. Now that we know the virus won’t follow us home on our shopping bags, that extreme PPE habits are actively harming the planet, and that the pandemic is likely on its way to becoming endemic, it’s imperative to decrease PPE use and develop waste-reduction strategies to ensure a healthier future for all.
“This is a moment,” Montgomery concludes. “I think the key will be what happens in the next year. Because there’s momentum, there’s energy, but if we don’t change our behavior, if we don’t change how we procure things, if we don’t change how we cost our PPE and other medical products to include that environmental and waste effort, we may miss the opportunity.”
 The Magazine of The Sierra Club
The Magazine of The Sierra Club